Hypercalcemia Headache- how to solve this puzzle?
Our Pet of the Month for May is little different from the ones we have done previously as we are sharing two different pets with similar, but not so similar stories while we dive into their clinical history.
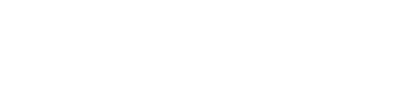
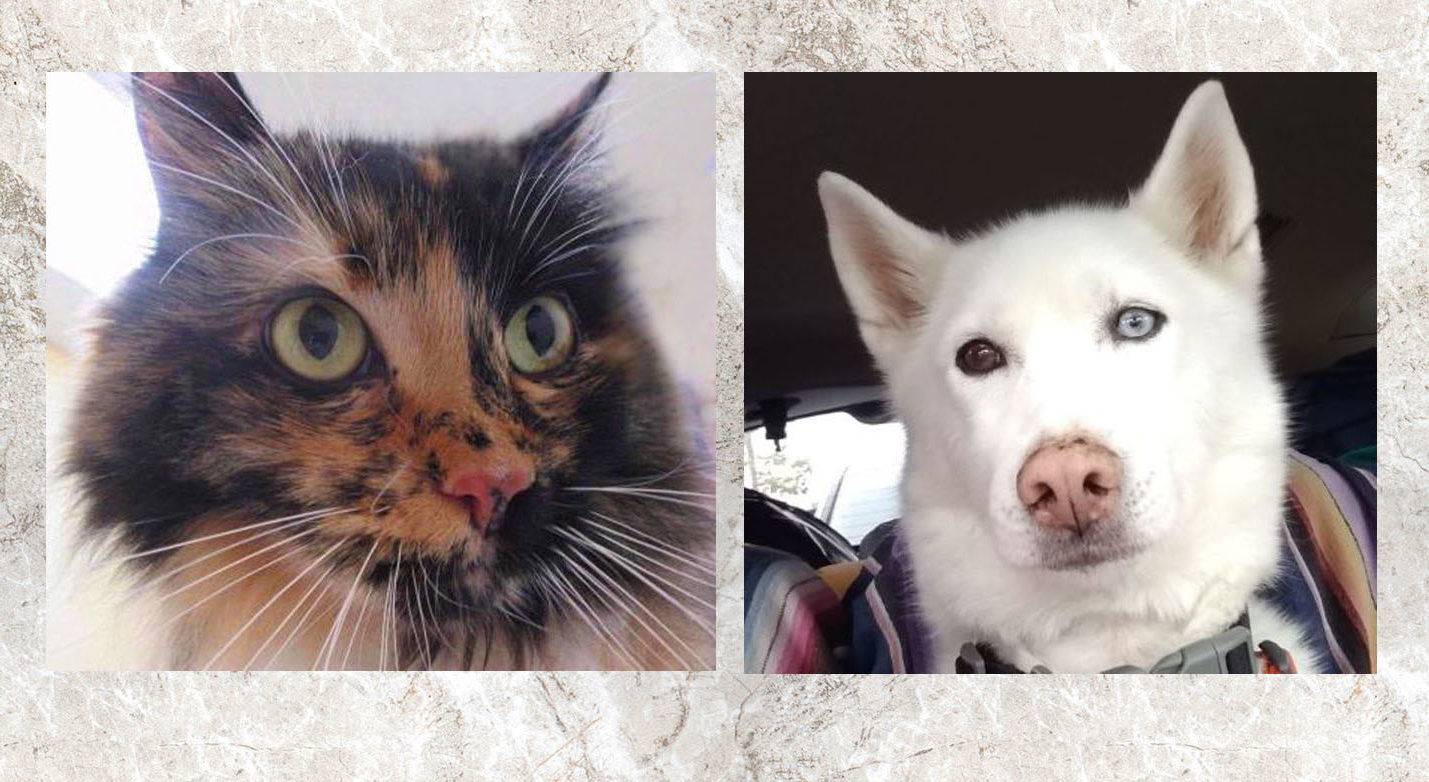
‘Glynnis Williams’, a cat and ‘Dakota’, a Siberian Husky were seen at Hawthorne Hills Veterinary hospital and both were diagnosed with elevated blood calcium levels. We pursued further diagnostics for each patient which led to a completely different diagnosis in each case. Hypercalcemia means elevated levels of the calcium in the blood. Hypercalcemia is frequently encountered in clinically normal patients based on routine pre-anesthetic or annual bloodwork. Calcium is an important electrolyte and responsible many processes in the body, and mild fluctuations may not be significant. The clinical signs associated with high blood calcium varies depending on the magnitude and duration of hypercalcemia. The most common clinical signs of persistently high calcium levels are polyuria (increased urination), polydipsia (increased thirst), lethargy, inappetence, and weakness.
The possible causes of increased calcium are numerous:
- Hyperparathyroidism-Over active parathyroid gland- This gland maintains Calcium and phosphorus balance in the body.
- Addisonian disease- deficiency of hormones produced by adrenal gland. Common in dogs compared to the cats.
- Renal disease- This alters calcium and phosphorus balance
- Hypervitaminosis D-This is a less common cause include high Vitamin D intake, dairy with Vit D in it and ingestion of certain house plants like day blooming Jasmine.
- Idiopathic hypercalcemia – more common in cats
- Osteolysis- bone lysis
- Neoplasia- Increased calcium due to Malignancy- It is one of the most common causes of increased calcium and can be seen in a variety of cancers including anal gland carcinoma in dogs, lymphoma, multiple myeloma etc.
- Fungal disease- certain fungal infections cause tissues to calcify, especially lung tissue, and cause elevated blood calcium levels
- Spurious- sample contamination/error, or age of the patient (calcium levels are higher in young dogs and large breeds who continue growing for up to 2 years of age)
Calcium is present within the circulation in three forms – ionized calcium which is the active form; protein-bound calcium and the chelated form complexed with lactate, citrate and bicarbonate. The first step in investigating high calcium is to check ionized calcium which is an active form of calcium that the body senses, responds to and is tightly regulated. If ionized calcium is normal, even if total calcium is increased, no further diagnostics are warranted.
If ionized calcium is high this confirms hypercalcemia, then next step is to identify underlying cause which is often challenging. The treatment of underlying cause is necessary to resolve the increased the calcium. By featuring both Glynnis and Dakota we want to highlight the importance of testing to get to the underlying cause of hypercalcemia in dogs and cats; knowing the cause helps ensure the appropriate treatment.
Below is the detailed discussion of each case.
Glynnis is a 16-year-old spayed female cat who was diagnosed with hyperthyroidism and underwent radioiodine treatment in 2018. Post treatment she became hypothyroid and was started on thyroid supplement. During the routine monitoring of thyroid levels it was noticed her calcium level was high. To confirm if it is truly elevated, ionized calcium was also checked and that also came back high. Results were conveyed to Glynnis’s owner along with the next steps to investigate the underlying cause. It was recommended to Glynnis have chest radiographs, abdominal ultrasound, and additional blood work to check parathyroid gland and any evidence of the cancer.
Chest radiographs- There were some age related changes in her lungs but no evidence of cancer
Abdominal ultrasound- Intestinal thickening was noted which could be suggestive of Inflammatory bowel disease or gastrointestinal neoplasia.
Malignancy Panel. This is a special test to check ionized calcium, parathyroid hormone (PTH) and parathyroid hormone – related protein ( PTHrP). Positive parathyroid hormone-related protein (PTHrP) result with high ionized calcium and concurrent suppression of parathyroid hormone (PTH) supports hypercalcemia of malignancy. Increased PTHrP concentrations have been reported in cats with carcinoma (pulmonary, renal, and thyroid), osteosarcoma, and occasionally lymphosarcoma. All three values came back normal including the ionized calcium.
Based on the above results it was concluded that Glynnis has idiopathic hypercalcemia with unknown cause. This is the most common cause of high calcium in cats and many cats are asymptomatic. The treatment for idiopathic hypercalcemia is supportive to lower the calcium levels rather than identifying and treating the cause. Glynnis was recommended to have fiber added to her diet to reduce the absorption of calcium from her intestines. This was started even before we did additional diagnostics and seemed to be working with normal ionized calcium on malignancy panel. We plan to recheck her ionized calcium again to monitor the response to the dietary therapy.
Dakota- is an 11-year-old spayed female Siberian Husky. She had been experiencing a decreased appetite and change in energy for several months before the owner brought her in. Due to Dakota’s appetite issues, she had lost weight, but her physical exam was fairly normal with the exception of moderate dental tartar. To understand the appetite change, we collected baseline blood work and a urine sample. We determined she had a urinary tract infection which was treated with a course of antibiotics. The blood work however, revealed a very high serum calcium level and an elevated SDMA (a marker of kidney function). We ruled out Addison’s disease based on a normal serum Cortisol level.
We started Dakota on medication to control any nausea she might be experiencing, an appetite stimulant to encourage her to eat, and a several easy to eat and digest foods to see if that helped her eat more consistently. Once we uncovered some kidney changes and the hypercalcemia, we advised transitioning her to a prescription kidney food that had balanced nutrition and controlled calcium levels.
To figure out the underlying cause of Dakota’s hypercalcemia, we:
- Confirmed the elevated calcium with additional testing sent to Michigan State Veterinary Diagnostic Lab – checking the PTH level, the Ionized Calcium and a Parathyroid Related Protein level – all of which confirmed our diagnosis of Primary Hyperparathyroidism.
- Scheduled her for chest & abdominal radiographs; fortunately, those images were considered normal.
- Arranged with a veterinary radiologist to perform an ultrasound evaluation of Dakota’s parathyroid glands; this confirmed a very large gland on the left side of her neck – consistent with Primary Hyperparathyroidism.
The treatment for Dakota’s hypercalcemia is to surgically remove the parathyroid gland. This can be a complicated surgery and her overall care needs to be managed closely to ensure that her calcium levels return to normal. We advised the owners that they needed to schedule an appointment with an internal medicine specialist first, and that individual would help manage Dakota’s care in conjunction with a veterinary surgeon specialist.
We consulted the internist about therapy pending Dakota’s scheduled appointments with the specialists. Dakota was started on Alendronate (Fosamax) to help lower her blood calcium. The medication cannot be given with any food and washed down with water (so a bit challenging to give) but Dakota was cooperative. The dose is then titrated up over time. The goal was to have her body pull the calcium back into her bones without spilling too much calcium in the urine, potentially causing bladder stones. As Dakota’s blood level started coming down, she was beginning to feel much better – more energy, and eating more consistently.
Dakota is waiting on her surgery, but her prognosis is good if all goes well. We look forward to her recovery.